Improving Health System Policy Making and Performance
for Better Health
for Better Health
|
An effective health system regardless of size or complexity (e.g. a large national system, a small public primary health network, or a private integrated network) protects its members from impoverishment (financial protection), ensures users and patients satisfaction, and engenders cross-sectoral policies that promote individual and public health beyond the realms of health care. Such highly performing health system ensures healthy population and individuals.
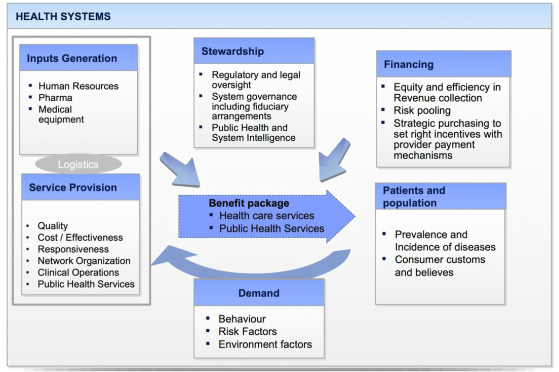
Although there are a number of different conceptual frameworks explaining what is a Health System and what are its objectives, most define it as all the resources, organizations, policies and people whose primary intent is to protect, improve, and rehabilitate the health of individuals and populations. Most also include four key components: Health System Financing; Health Services Provision; Benefit Package, and Health System Stewardship and Regulation (i.e. regulation, system intelligence, governance, surveillance, multi sector engagement for health). Both the specific design of each of these four components and the harmonic interplay among them defines the performance of the system. Health Systems aim at protecting and improving health, provide financial risk protection from illness (that members of society do not face impoverishing when facing illness), and that they achieve it with the satisfaction of legitimate expectations of the population and in a financially sustainable way for the system and the country. Health Systems performance is a core area of analysis, work and advice of the CHD. We provide advice and training as well as support health system leaders, donors and policy makers in all four key pillars of Health Systems: Health Financing, Health Service Provision, Benefit package, and Stewardship-Regulation, including the systemic interplay of the system functions for optimum health system performance. |
Defining the Health System Architecture and Transition Strategies
A key determinant of optimal system performance is ensuring the coherence of all system functions with the country health system objectives (or subsystem objectives), the benefits package, the health financing components, the service provider capabilities, and the management framework, and regulatory framework.
Ensuring the coherence in the design and implementation of all system components either at initial launch (seldom the case) or at the transition from an existing system (often the case) is as important as, or more important than, selecting specific options and designs for each component of the system. It requires a comprehensive design and optimization of the Health System with all its components at the national, subnational, or private integrated systems. The most common mistake in health systems reform and transformation is the belief that reforming only one function of the system (financing, provision, regulation, entitlements) would render the expected results. As expected in a system equilibrium, even if the emphasis is on one function of the system, adjustments are likely to be required in the other functions to succeed. CHD is particularly distinctive in its ability to support policy makers and system leaders in comprehensive system architecture design, implementation and transformation |